Are you concerned about your bone health and want to know how your diet plays a role in preventing osteoporosis? In this article, we will explore the important connection between osteoporosis and diet, and provide you with valuable insights and tips on what you should know to keep your bones strong and healthy. Discover how certain nutrients, like calcium and vitamin D, are essential in supporting bone density, and learn about the best food sources to incorporate into your daily diet for optimal bone health. Say hello to stronger bones by taking simple dietary measures!

Understanding Osteoporosis
Osteoporosis is a condition characterized by weak and brittle bones. It occurs when the body loses too much bone, doesn’t make enough bone, or both. As a result, bones become thin and fragile, making them more prone to fractures. Osteoporosis is often called the “silent disease” because it develops gradually and without noticeable symptoms until a fracture occurs.
Causes of Osteoporosis
There are several factors that can contribute to the development of osteoporosis. Age is a significant factor, as bone density naturally decreases as we get older. Hormonal changes, such as menopause in women, can also lead to bone loss. Other causes include a family history of osteoporosis, certain medical conditions like rheumatoid arthritis and celiac disease, and the use of certain medications like corticosteroids.
Risk Factors for Osteoporosis
Certain factors can increase your risk of developing osteoporosis. Women are more likely to develop the condition compared to men, especially after menopause. Age, as mentioned earlier, plays a role as well. Individuals with a family history of osteoporosis, a small and thin body frame, and a history of fractures are also at a higher risk. Additionally, lifestyle factors such as a sedentary lifestyle, smoking, excessive alcohol consumption, and a poor diet can contribute to the development of osteoporosis.
The Role of Diet in Osteoporosis
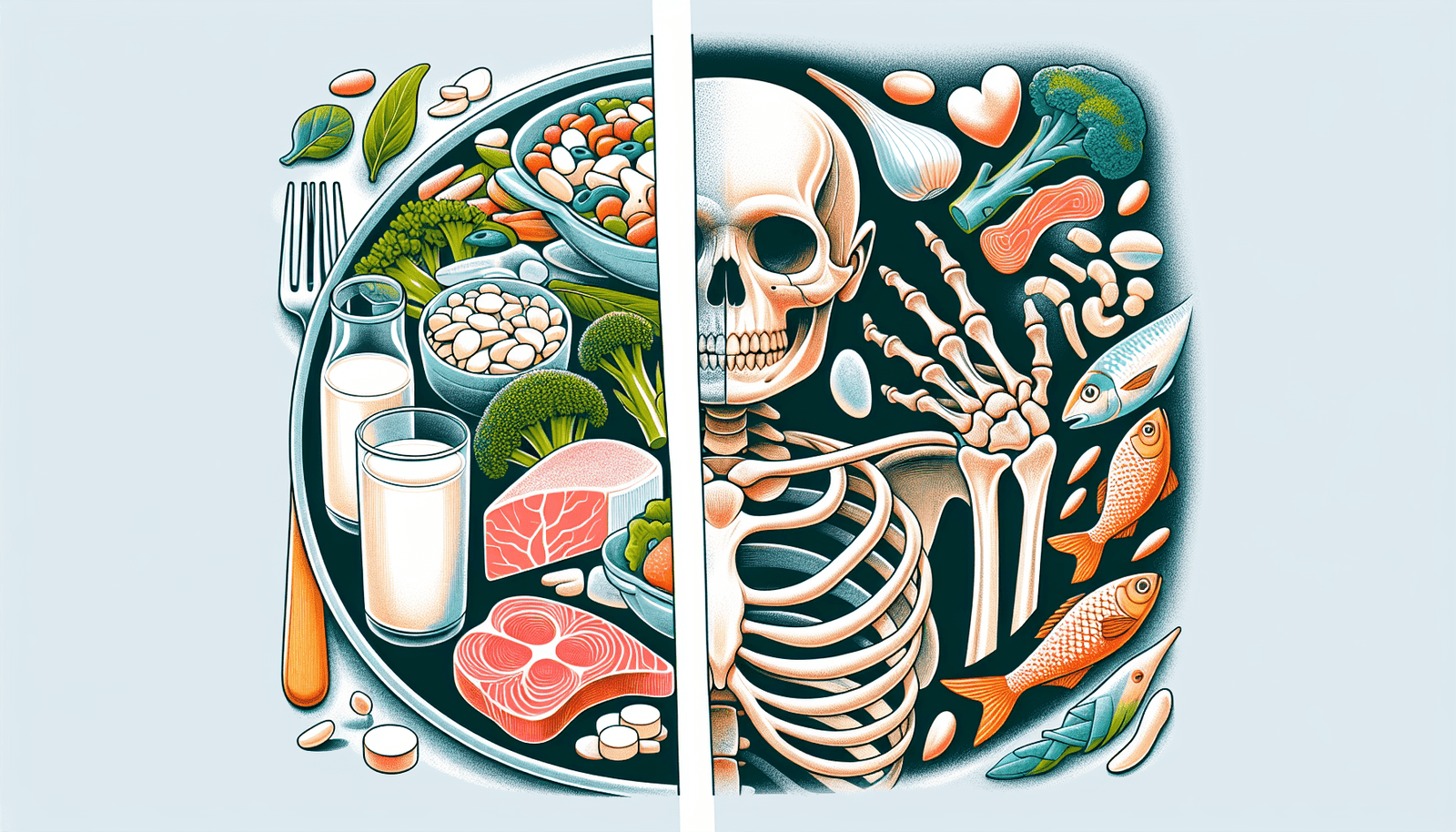
Nutrition plays a crucial role in maintaining strong and healthy bones. A well-balanced diet that provides adequate amounts of key nutrients is essential for preventing and managing osteoporosis.
Importance of Nutrition in Bone Health
Adequate nutrition is necessary for the body to build and maintain healthy bones. Our bones rely on nutrients like calcium, vitamin D, protein, and various minerals to stay strong and resilient. Without these essential nutrients, bones can become weak and porous, increasing the risk of fractures.
Key Nutrients for Strong Bones
Calcium, vitamin D, and protein are key nutrients that play a vital role in bone health. Calcium is the primary component of bone tissue and is essential for maintaining bone density. Vitamin D helps the body absorb calcium and supports bone mineralization. Protein is necessary for building and repairing bone tissue.

Dietary Factors that Affect Bone Health
While consuming adequate amounts of key nutrients is important, certain dietary factors can negatively impact bone health. Excessive intake of sodium, caffeine, and alcohol can interfere with the body’s ability to absorb and utilize calcium. Additionally, certain compounds like oxalates and phytates found in certain foods can inhibit calcium absorption.
Calcium and Vitamin D
The Importance of Calcium in Bone Health
Calcium is a vital nutrient that contributes to the maintenance of strong and healthy bones. It serves as a building block for bone tissue, helping to maintain bone density and strength. Adequate calcium intake is crucial throughout life, but it becomes even more important during childhood and adolescence when bones are growing rapidly.
Sources of Calcium
Calcium-rich foods include dairy products like milk, cheese, and yogurt, as well as leafy green vegetables such as broccoli, kale, and spinach. Other sources of calcium include tofu, almonds, sardines, and fortified foods like soy milk and orange juice.
Recommended Daily Intake of Calcium
The recommended daily intake of calcium varies depending on age and gender. For adults aged 19-50, the recommended intake is around 1000 mg per day. However, for women over 50 and men over 70, the recommended intake increases to 1200 mg per day.
Vitamin D and its Role in Calcium Absorption
Vitamin D is essential for the absorption and utilization of calcium in the body. Without sufficient vitamin D, the body cannot effectively absorb the calcium consumed through diet. Adequate sun exposure and consumption of foods rich in vitamin D, such as fatty fish, fortified dairy products, and eggs, can help ensure optimal vitamin D levels.
Sources of Vitamin D
The primary source of vitamin D is sunlight. When exposed to sunlight, the skin produces vitamin D. However, it can also be obtained through dietary sources such as fatty fish like salmon and mackerel, egg yolks, fortified milk and orange juice, and certain types of mushrooms.
Recommended Daily Intake of Vitamin D
The recommended daily intake of vitamin D varies depending on age. For most adults, including those over the age of 70, the recommended intake is around 600-800 international units (IU) per day. However, individuals with osteoporosis or other specific health conditions may require higher doses as recommended by their healthcare provider.
Protein and Osteoporosis
The Impact of Protein on Bone Health
Protein is a crucial nutrient for bone health as it provides the structural framework for bones and helps in the bone remodeling process. Adequate protein intake is essential for maintaining bone mass and preventing bone loss.
Recommended Protein Intake for Bone Health
The recommended protein intake for adults is around 0.8 grams of protein per kilogram of body weight. However, for individuals with osteoporosis or those at risk of bone loss, a slightly higher intake of protein may be beneficial. Including protein-rich foods such as lean meats, poultry, fish, legumes, and dairy products can help meet protein needs and support bone health.
Sources of High-Quality Protein
High-quality protein sources include lean meats like chicken and turkey, fish such as salmon and tuna, eggs, dairy products such as milk, yogurt, and cheese, as well as plant-based sources like legumes, tofu, and quinoa.
Oxalates and Phytates
Understanding Oxalates’ Effect on Calcium Absorption
Oxalates are naturally occurring compounds found in certain foods that can bind to calcium and form insoluble crystals. This can interfere with calcium absorption and increase the likelihood of calcium being excreted from the body. Foods high in oxalates include spinach, rhubarb, beet greens, and nuts.
The Role of Phytates in Reducing Mineral Absorption
Phytates are compounds found in certain plant-based foods. They have the ability to bind to minerals like calcium, zinc, and iron, forming complexes that are poorly absorbed by the body. Foods high in phytates include whole grains, legumes, and nuts.
Foods High in Oxalates and Phytates
While foods high in oxalates and phytates can be healthy choices overall, individuals with osteoporosis or at risk of calcium deficiency should consume them in moderation. It is important to note that individuals who follow a varied and balanced diet typically do not need to be overly concerned about the impact of oxalates and phytates on calcium absorption.
Sodium and Osteoporosis
The Relationship between Sodium and Bone Health
Excessive sodium intake can increase calcium excretion through urine, leading to bone loss over time. High levels of sodium in the diet can disrupt the balance of calcium in the body, making bones more susceptible to becoming weak and brittle.
Recommended Sodium Intake for individuals with Osteoporosis
The American Heart Association recommends limiting sodium intake to no more than 2,300 milligrams (mg) per day, preferably aiming for an intake of 1,500 mg or less for individuals with osteoporosis or hypertension.
Foods High in Sodium
Foods high in sodium include processed and packaged foods such as chips, fast food, canned soups and vegetables, deli meats, and pre-packaged meals. It is important to be mindful of sodium content when making food choices and opt for fresh and minimally processed options whenever possible.
Alcohol and Osteoporosis
The Negative Impact of Alcohol on Bone Health
Excessive alcohol consumption can have a detrimental effect on bone health. High alcohol intake interferes with the body’s ability to absorb calcium, impairs vitamin D metabolism, and disrupts the normal balance of bone formation and breakdown, leading to decreased bone density and increased fracture risk.
Recommended Alcohol Consumption Guidelines for Individuals with Osteoporosis
For individuals with osteoporosis, it is recommended to limit alcohol consumption. Women should aim for no more than one alcoholic drink per day, while men should aim for no more than two drinks per day. It is important to note that even moderate alcohol intake can have negative effects on bone health, and individuals with osteoporosis may want to consider avoiding alcohol altogether.
Caffeine and Osteoporosis
The Effects of Caffeine on Calcium Absorption
Caffeine is a natural stimulant found in coffee, tea, chocolate, and some carbonated beverages. While caffeine itself does not directly cause osteoporosis, excessive caffeine intake can interfere with calcium absorption, especially when consumed in conjunction with low-calcium diets. However, moderate caffeine intake does not appear to have a significant impact on bone health.
Recommended Caffeine Intake for Bone Health
Moderate caffeine intake is generally considered safe and does not significantly affect bone health. It is recommended to consume no more than 400 milligrams of caffeine per day, which is roughly equivalent to 4 cups of brewed coffee or 10 cans of caffeinated soda. It is important to consider the overall dietary calcium intake when consuming caffeine-containing beverages.
The Mediterranean Diet
Overview of the Mediterranean Diet
The Mediterranean diet is a traditional eating pattern followed in countries bordering the Mediterranean Sea. It emphasizes the consumption of fruits, vegetables, whole grains, legumes, nuts, seeds, fish, and olive oil, while limiting the intake of red meat, processed foods, and sweets.
The Benefits of the Mediterranean Diet for Bone Health
The Mediterranean diet is often associated with numerous health benefits, including improved bone health. It provides a variety of nutrients necessary for maintaining healthy bones, such as calcium, vitamin D, and magnesium. Additionally, it is rich in antioxidants and anti-inflammatory compounds, which may help reduce the risk of bone loss and fractures.
The Role of Supplements
When Supplements Might Be Necessary
While obtaining nutrients from a well-balanced diet is ideal, supplementation may be necessary in certain cases. Individuals who have difficulty meeting their nutrient needs through diet alone or those with specific medical conditions that affect nutrient absorption may benefit from supplements. It is important to consult with a healthcare professional before starting any supplements.
Common Supplements for Osteoporosis Prevention and Treatment
Common supplements used for osteoporosis prevention and treatment include calcium and vitamin D supplements. Calcium supplements are available in different forms, such as calcium carbonate and calcium citrate. Vitamin D supplements can be found in various strengths and formulations. Other supplements, such as magnesium, vitamin K, and omega-3 fatty acids, may also be recommended based on individual needs and circumstances.
In conclusion, proper nutrition plays a vital role in maintaining strong and healthy bones. Consuming a well-balanced diet that includes adequate amounts of calcium, vitamin D, and protein, while minimizing the intake of sodium, caffeine, and alcohol, can help prevent and manage osteoporosis. Additionally, adopting a Mediterranean-style eating pattern and, if necessary, considering the use of appropriate supplements can further support bone health. Remember, it’s never too early or too late to start taking care of your bones, and making informed dietary choices is an important step towards ensuring optimal bone health throughout life.